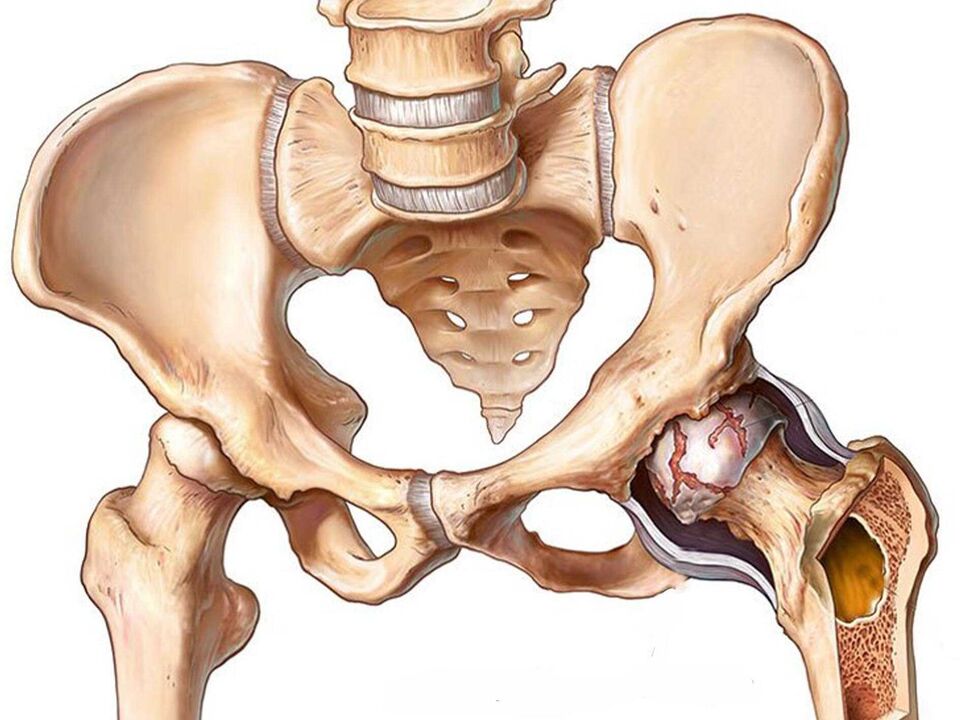
hip disease(hip joint disease) is a joint deforming arthropathy, a chronic, non-inflammatory disease that affects the hip joints (one or both at the same time). The disease is characterized by degenerative dystrophy. This means that the cartilage that forms the hip joint undergoes degenerative changes, as well as changes to the surface of the bone. In addition, bone growths (osteophytes) form, joints deform, the amount of movement in the affected joints is reduced, and they become very painful and uncomfortable.
The hip joint is one of the largest joints in our body. Thanks to him, the human body performs a very important motor function, and he is also responsible for ensuring that our bodies move. If the hip is ill, then this affects the entire body, making it impossible for a person to live peacefully, walk, let alone exercise. We often see older adults forced to rely on crutches due to hip disease.
Although the hip joint is very large and strong, it is also fragile, especially over time. Hip pain can significantly reduce the quality of life in humans.
Hip disease (arthropathy of the hip joint)After knee joint disease (knee joint disease), the frequency of confirmed cases ranks second in joint disease.
Classification of hip arthropathy (arthropathy of the hip)
it happenship diseaseprimary and secondary.
- The etiology of primary hip disease is mainly the inevitable wear and tear of the hip joint over the life course, usually affecting people after the age of 40.
- The causes of secondary hip arthropathy are usually the following diseases: congenital femoral dislocation, osteonecrotic mass of the hip in its head region, Peter's disease, early hip trauma, inflammatory disease of the hip. inhip joint diseaseA joint can be affected individually, or both joints can be affected at the same time.
There are several types of hip disease:
- Dysplasia (is a congenital condition characterized by joint dysplasia).
- Involution (typical in older age groups, associated with age-related changes).
- After infection (previously purulent or suppurative allergic rheumatoid arthritis).
- Disease due to Peters disease (development of osteochondrosis of the femoral head).
- hip diseaseDue to trauma (neck and head (femur) fractures).
- Hip disease due to metabolic disorders (metabolism).
- Dishormonal (long-term use of corticosteroids, antidepressants).
- Idiopathic (the cause of which cannot be determined).
Symptoms of hip disease (hip disease)
In order to correctly describe the symptoms of hip arthropathy, the stage of the disease should also be considered, as the symptoms depend on the stage of the disease.
Stages of Hip Arthropathy (Hip Arthropathy)
In general, hip arthropathy (hip disease) is divided into three stages:
- The first stage of hip disease. This is the initial stage of the disease and symptoms are still mild. The joints at this stage are not sore, and soreness occurs only after physical exertion, such as lifting heavy objects or jogging, long-distance travel, etc. After the person rests, the pain disappears. For example, patients may also experience lameness if they walk more than two kilometers. Increased soreness going up stairs. The motion volume of the joint is slightly reduced or remains the same. X-rays can only show small changes in bone structure.
- Stage 2 of hip disease. This stage develops without first stage treatment. In addition to the above symptoms, there is also an increase in specific cracks (crunching) in the joints. The soreness becomes more intense and begins to radiate to the groin area and can also spread to the thighs and knees. At this stage, not only is it strong, but any movement can cause symptoms of pain, even a slight load on the hip joint. Even getting up or turning the trunk can cause pain. Tension in the muscles around the joints does not go away even at night, so patients often complain of pain in the thighs at night. A person may begin to limp even after taking small steps (up to 500 meters). At this stage, the disease has forced a person to rely on crutches when walking. Limitations of joint movement become more pronounced. The presence of osteophytes is identified based on the diagnostic X-ray results.
- The third stage of hip disease. The final stage of the disease. During this stage, the pain becomes permanent and afflicts the patient. Any movement, even the weakest, can increase pain symptoms several times over. At this stage, the hip joint is fully immobilized. Loss of muscle mass in the thighs and buttocks is very noticeable due to muscular dystrophy. The characteristic is that the patient cannot stand directly, and the body will be skewed. Any arthropathy can lead to the formation of contractures (flexion positions), in which case the contractures also develop due to a state of constant tension on the muscle fibers, and the leg on the affected side becomes shorter. Due to the immobilization of the hip joint, the entire leg ceases to perform its motor functions, which has very negative effects and leads to their osteochondral lesions. In addition, the spine is also affected, with discomfort and pain in the sacral area.
Causes of hip disease (hip disease)
Main causes of hip disease:
- Age-related changes in joints. Typical old man. The hip joint wears out over time, stops performing its function over time, and "dries up, " which causes its shock-absorbing function and the friction between the bones that form the joint to decrease.
- Hip injury. The most common injury in this age group is a femoral neck fracture, which can lead to disability without proper treatment. Joints can be injured at any age, but older adults are more prone to injury.
- Metabolic disorders. This is typical for people with a history of metabolic disorders and disorders associated with impaired metabolism.
- Violation of hormonal status. More female characteristics, especially in women who have been taking antidepressants and glucocorticoids for a long time.
- Genetic abnormalities in the development of the musculoskeletal system, as well as congenital abnormalities. Unfortunately, at present, a considerable number of children are born with congenital musculoskeletal and neurological disorders. As for abnormalities in the development of the hip joint, this may include its dysplasia, in which several structures of the joint are not developed.
- Systemic arthritis. Injuries to multiple joints can also lead to damage to the hip joint. In this case, one of the main risk factors would be the presence of inflammatory processes.
- Rheumatism and chronic arthritis. All of these can also cause pain in the hip joint. Such diseases causing joint pain in the study include: rheumatism; rheumatoid arthritis; spondyloarthropathy; juvenile rheumatoid arthritis.
- Failure of osteochondrosis. Osteochondrosis of the spine is a fairly common and serious disease that "destroys" other structures in our body besides the spine, especially the hip joints.
- Muscles and ligaments of joints. Damage to these structures may also be the result of hip degenerative and dystrophic processes.
- Infectious lesions of the joint itself and the femur. Such lesions are very serious because they can have serious consequences and are sometimes difficult to treat. Osteomyelitis can occur, which simply "eats" or "dissolves" bone tissue. Tuberculous lesions may also occur, and this localization is more common in prepubertal children. A pelvic abscess, which is often the result of an untreated or poorly treated infectious process, such as appendicitis, an inflammatory process, especially when the female reproductive organs are involved (ovarian disease), the development of an abscess that deepens in the ischiorectal area, leading to impaired gait(limp). In most cases, pain and lameness are the result of compression or damage to a nearby nerve (sciatica or obturator).
- malignant tumor. Malignant tumors rarely affect the hip joint and the surrounding bones, as the cause of the disease is more commonly metastasis from other malignant areas, such as breast or lung cancer.
- The lumen of the aorta and iliac arteries are narrowed (their stenosis and occlusion). At the same time, the joints receive less and less of the nutrients they need to function properly, causing them to degenerate.
Risk groups for hip disease (hip disease)
Major risk groups can include the following categories of people and harmful factors:
- elderly. The disease is typical of the elderly for the elderly because the degenerative process happens at this age.
- female. According to statistics, women are more prone to hip problems.
- People who are overweight or obese.
- Previous trauma to one or both hip joints.
- Genetic susceptibility to this disease and congenital abnormalities in hip development.
- There were previous infectious lesions, such as abscess, aseptic necrosis of the femoral head, osteomyelitis, etc.
- Hard physical labor.
- Summer residents are at an extremely high risk of developing hip disease.
Prevention of hip joint disease (hip disease)
The main measures to prevent hip joint disease are as follows:
- There is a dose of physical activity. It is important to perform gymnastics and kneading of the joints to prevent the development of their pathological processes and their slower aging. This not only helps improve the condition of the hip joint, but also the entire body.
- If there is a metabolic disorder, it should be corrected. For this, you should contact a specialist.
- Pay attention to your weight. Don't forget that the hip joint is already under a lot of load, almost the entire body, so you shouldn't interfere with it to perform its function. Also, a lot of weight can put so much pressure on the joints that they gradually collapse. People who are overweight are also prone to metabolic disorders.
- Avoid sharp turns, especially if you're not warmed up and unprepared, this will prevent you from injuring the head and neck of the femur.
- Of course, it's best to choose sports that pose the least risk of joint damage, such as swimming or yoga, especially if there is a genetic predisposition or developmental abnormality.
- A susceptibility to joint diseases means handling them with care, as well as regular visits to the doctor, so as not to miss out on a disease that may develop or any other pathological process in the joint.
- If a child is diagnosed with hip dysplasia, it should be treated immediately! It is better to have a child immobilized for a few weeks at an early age than to suffer for a lifetime.
- Treat infectious diseases promptly, especially those that may spread to the hip joint.
Diagnosis of hip joint disease (hip disease)
When diagnosing hip disease, it's important to find out what's causing it. After all, as we've discussed above, there are many reasons, they are varied, andHip Osteoarthritis Treatment, respectively will be fundamentally different. Sometimes it's not easy, sometimes it's not at all. The focus is on studying the presentation of the disease and selecting an appropriate treatment.
First, the doctor will carefully ask the patient to study in detail the main complaint, the cause of the disease, the genetic burden, the presence or absence of injury, etc. It is important to understand the above-mentioned complaints and when they were observed in the patient.
After the interview, the doctor personally examines the affected area for inflammatory changes, nutrition, deformities, shortened limbs, asymmetry, etc. And children may experience "clicking" symptoms.
An important point is the additional examination methods - computer and magnetic resonance imaging, ultrasound and X-ray examinations as they will help to make the final diagnosis. This item is extremely important in the differential diagnosis of hip joint disease from other hip joint diseases.













































